Climate change is a ‘health’ issue, described by the World Health Organisation as the greatest threat to human health we will ever face. However, tackling it offers the single greatest opportunity to improve human health we will ever have.
Medicines use accounts for 25% of the NHS’s carbon footprint, which is itself responsible for approximately 5% of the UK’s carbon footprint, and so optimising medicine protects the environment and simultaneously protects our patients, our colleagues and every single member of our community.
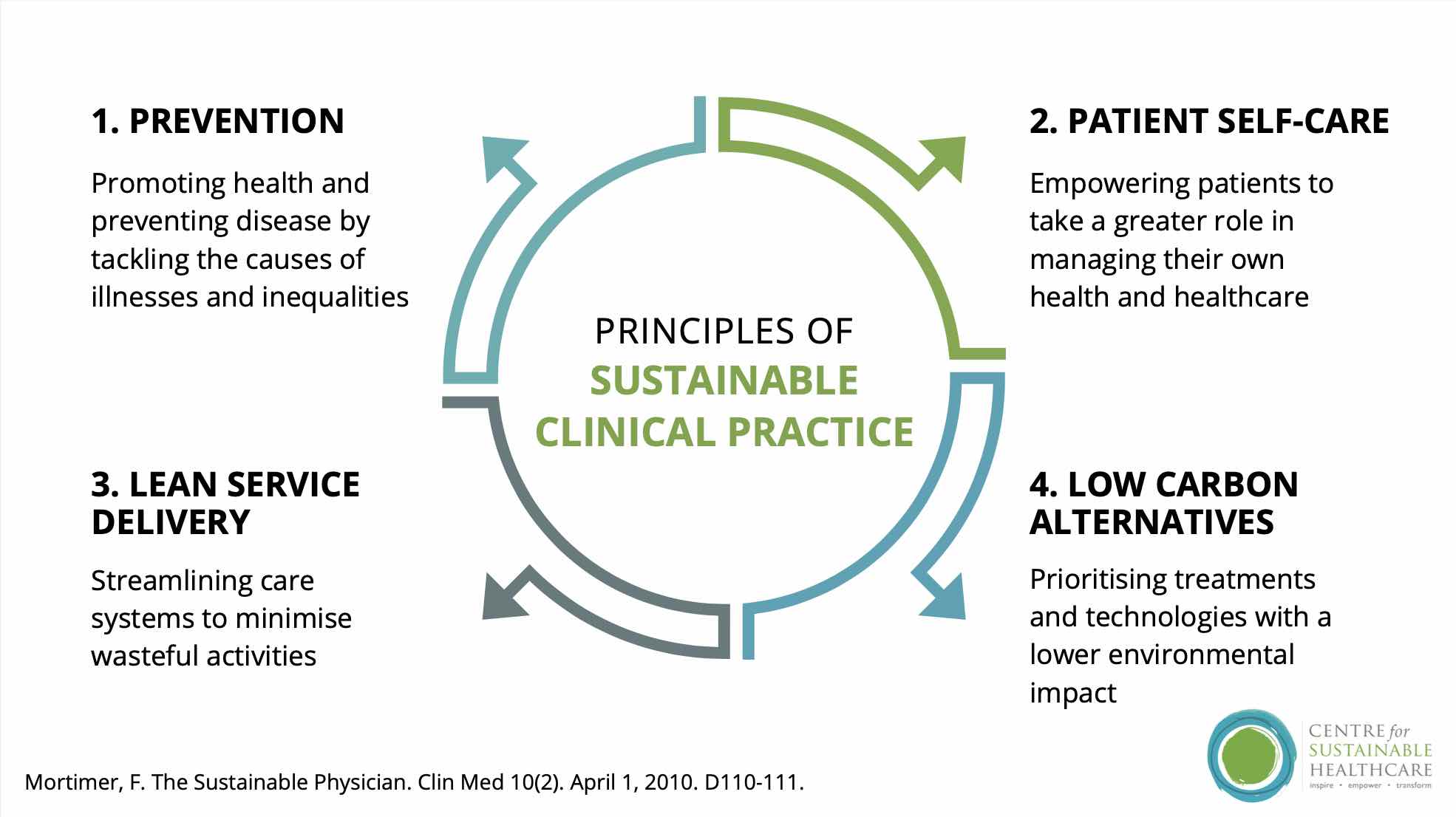
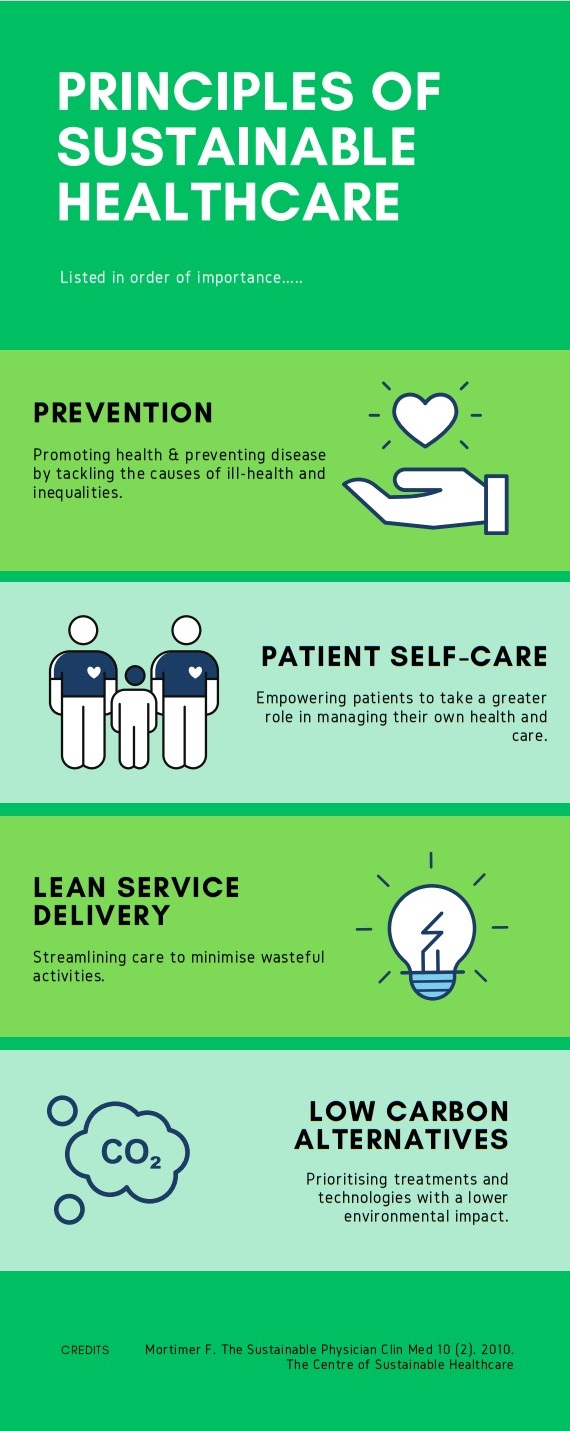
There are 4 principles of Sustainable Healthcare, ranked in order of importance.
- Prevention of ill-health/Promotion of good health
- Patient Empowerment to Self-Care
- Lean Service Delivery
- Low Carbon Alternatives
We are incredibly proud of our progress, however we are always delighted to champion new projects, sharing success across the region. If you want to know more or have any other questions, please get in touch via medicine.question@nhsdorset.nhs.uk
Respiratory Medicines
Pharmacy respiratory green agenda and sustainability
In this video:
Resources
Greener Practice: what is asthma and how to treat it?
Greener Practice: inhaler device types for asthma
Recycling
Blister pack recycling – this is currently available in selected Boots and Superdrug pharmacies.
PenCycling – PenCycle is a recycling scheme run by the pharma company NovoNordisk for their diabetes, weight management and growth hormone pens. Community Pharmacies can set themselves up as a recycling hub, or patients can recycle their own pens directly. Full information here.
(But remember! Medicines that aren’t needed, don’t need to be recycled. Always think “Health Optimisation” as a first step!)
KidzMed Pill School
Liquid medications are less sustainable and have more ecological impacts than tablets/capsules (they weight more and so more energy is needed when transporting and disposing of them. Conversely, tablets or capsules tend to contain less sugar than liquid medicines, are easier to source, transport and store, and are associated with less waste, so are good for patients, carers and pharmacies as well as the environment).
In 2018, charity Pharmacy Research UK and the Evelina London Children’s Hospital undertook a project to teach young patients how to swallow tablets. This led to the launch of the award-winning KidzMed Pill School at the Great North Children’s Hospital, Newcastle.
Poole Hospital’s paediatric department now runs ‘Pill School’ classes which are accessible to any child in Dorset. Email paediatricpharmacists@uhd.nhs.uk for information on class times and availability.
Pharmaceutical Waste Management
Pharmaceuticals in the environment is a growing problem, but one that we can tackle. Drugs taken by humans and animals find their way into rivers, lakes and even drinking water, and can have devastating effects on the environment and human health.
There are three main ways that pharmaceuticals make their way into the environment:
- The biggest contribution comes from drugs taken by people or animals that are then excreted in urine or faeces – up to 90% of the active ingredient and the metabolites of many drugs can remain active in the environment after being excreted
- Improper disposal of drugs also makes a contribution — all pharmaceuticals should be returned to a pharmacy for proper disposal. When people throw the leftover drugs in the sink, down the toilet or into general rubbish, drugs end up in sewage treatment plants and wastewater. Commonly found contaminants include anti-inflammatories, sex hormones and antibiotics
- Some drug manufacturing facilities have also been shown to release active ingredients into nearby waterways, creating localised hotspots of pharmaceutical pollution
The most effective solutions are to prevent the need for medication waste through health promotion and medicines optimisation efforts (which will also reduce the volume of plastic waste produced), as well as educating patients about returning all unwanted drug doses to their pharmacy. Health care professionals can also ensure that drug disposal bins are used, regardless of sector. University Hospitals Dorset NHS Trust have produced a flow-chart guidance document explaining best practice, based on NHS England HTM recommendations for disposal of healthcare waste. A logo-less version for local adaptation can be obtained – please email tracy.lyons@nhsdorset.nhs.uk
Education
Knowledge is power! We want all Dorset healthcare professionals to be able to make the best decisions in terms of our patients and our planet. There is a world of information available to staff keen to know more about environmental sustainability and health, but to get you started, we’ve listed information on 4 brilliant free resources to start your journey today.
Monthly ‘Introduction to Medicines Sustainability’ sessions
45-60mins via Microsoft Teams. Learn about the health impacts of climate change, how health care delivery can make a difference, the principles of sustainable healthcare and hear about some of the fantastic work already taking place in Dorset. 2023 sessions are listed, email tracy.lyons@nhsdorset.nhs.uk to confirm a space.
- October, Monday 16th 12noon
- November, Tuesday 14th 1pm
- December, Friday 15th 12noon
Environmentally Sustainable Healthcare module
Environmentally Sustainable Healthcare – elearning for healthcare
The Environmentally Sustainable Healthcare (ESH) programme was developed with the Centre for Sustainable Healthcare and the HEE Northeast Faculty of Sustainable Healthcare to provide the healthcare workforce with the knowledge and skills to deliver healthcare for financial, social and environmental sustainability. There are 3 sessions in the Environmentally Sustainable Healthcare programme. Sessions 1 (Building a Net Zero NHS) and 2 (Environmental Sustainability in Quality Improvement) are suitable for all in the NHS healthcare workforce. Session 3 has been designed for the dentistry profession (Environmental Sustainability in Dentistry).
Greener NHS
The Greener NHS programme is spear-heading the NHS England road to Net Zero. This page outlines the national ambition, how to take action and showcases examples of system progress.
Climate and Health
From the UK Government office of Health Improvement, this resource helps health and care professionals prevent ill health and promote wellbeing as part of their everyday practice. It is designed to help frontline health and care professionals use their trusted relationships with patients, families and communities to reduce the contribution of the health and care system to the climate crisis.
Centre for Sustainable Healthcare
Since 2008 the Centre for Sustainable Healthcare has engaged healthcare professionals, patients and the wider community to understand the connections between health and environment and reduce healthcare’s resource footprint. The CSH offers (paid) education & training, free resources (including Sustainability in Quality Improvement) and free Sustainable Healthcare Networks for different professions/sectors.
Their work is guided by the principles of sustainable healthcare.